EHR Integration: The Definitive Guide
EHR Integration: What is it?
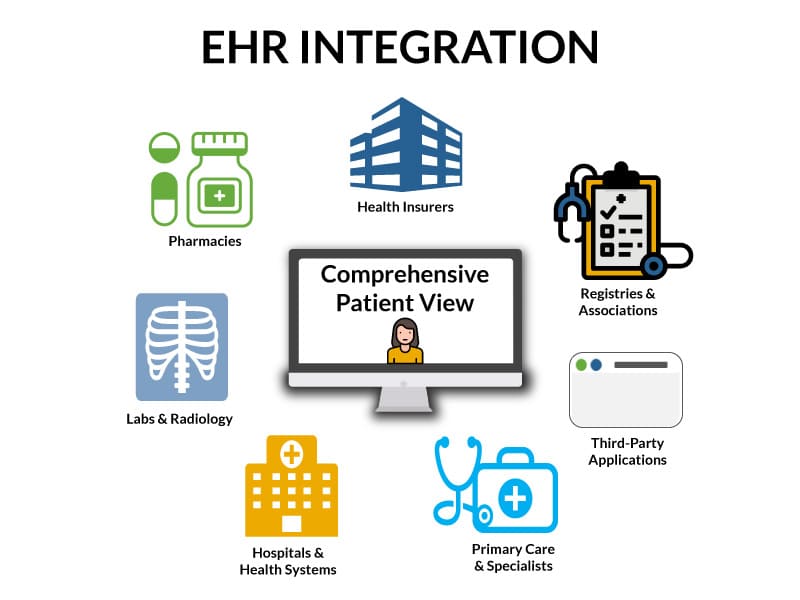
Electronic Health Records (EHRs) have revolutionized the healthcare landscape, transforming the way patient information is documented, accessed, and shared among healthcare providers. In this digital era, the integration of EHR systems plays a pivotal role in enhancing the efficiency and effectiveness of healthcare delivery. At its core, EHR integration refers to the seamless interoperability between different EHR systems, healthcare applications, and related technologies. It is the process of ensuring that diverse healthcare software solutions can communicate, share data, and work cohesively to provide a comprehensive view of a patient’s medical history and care journey.
Why is EHR integration critical to improving patient care?
Without EHR integration, we would have the same fundamental issue we’ve had with paper records – islands of disparate data and providers making healthcare decisions without complete visibility into the patient’s medical information. EHR integration enables the aggregation of comprehensive patient information from various sources into a single, unified record. This includes medical history, lab results, imaging reports, medications, and treatment plans. Having a holistic view of a patient’s health data allows healthcare providers to make well-informed decisions. More holistically, patient data from diverse sources can be aggregated and analyzed. This helps providers identify at- risk populations, implement preventive measures, and improve overall community health outcomes.
Benefits of EHR Integration
The sharing of patient information benefits patients and our healthcare system in the following key ways:
- Improves the quality of patient care. Providers can make better clinical decisions by having access to a patient’s complete medical record.
- Enhances care coordination. Patients with both acute and chronic conditions may receive care from a variety of different provider types. Healthcare providers may include hospitals, primary care providers, various specialists, skilled nursing facilities, and home care, to name a few. The handoffs between these different organizations require each to be familiar with the current episode of care and other aspects of the patient’s medical history.
- Reduces errors. By minimizing manual data entry and automating processes, EHR integration helps reduce the likelihood of errors associated with transcription and data duplication. This contributes to enhanced patient safety.

Approaches to EHR Integration
Historically, there have been two different EHR system integration methods:
1. APIs (Application Programming Interfaces)
APIs are digital bridges facilitating communication and data exchange between different software applications. In the context of EHR integration, APIs play a pivotal role in enabling interoperability between diverse health IT systems, such as lab portals, billing systems, remote patient monitoring applications, etc. APIs follow standardized protocols, ensuring consistent and secure data exchange, which provides the ability to connect EHR systems with various third party applications and exchange data in real time. Unfortunately, API capabilities are specific to each EHR vendor – meaning that you can only extract and insert the data elements that each EHR vendor includes in their API.
2. Direct Database Integation
For on-premise EHR systems, integrations can be done by connecting directly to the database. One important benefit of direct database integration is that you can access all of the information in the database, including data that may not be available to extract via API. Unfortunately, there are also some downsides. A detailed understanding of the database schema is required to extract the desired data. In addition, inserting data directly into the database is very risky due to the potential for corruption. For this reason, most EHR vendors consider it a violation of their contract to insert data directly into the database. Consequently, database integrations are limited to data extraction and are generally not bidirectional.

Emerging Trends in EHR Integration
Several key rules passed by the Office of the National Coordinator (ONC) in recent years are helping to drive new standards and innovations that improve EHR integration.
1. Fast Healthcare Interoperability Resources (FHIR)
FHIR is a standardized framework that defines how healthcare data can be exchanged between different health IT systems. Developed by the healthcare standards organization HL7, FHIR leverages the simplicity and flexibility of web-based technologies, such as RESTful APIs, making it a robust and widely adopted standard for data exchange in the healthcare domain. Its modular and resource-centric approach allows for the seamless integration of health information, enabling healthcare providers to access and share patient data more efficiently and securely. FHIR’s growing prominence stems from its ability to adapt to evolving technological trends, making it a pivotal component in the quest for a more connected and interoperable healthcare ecosystem.
2. Patient Access to Health Data
Due to ONC rule-making, health IT developers and healthcare providers must now enable patients to access their data through third-party applications via open APIs.
3. Robotic Process Automation
As mentioned above, EHR integrations via API and database suffer from various limitations. If the “back end” integration options don’t support the desired capabilities, why not integrate via the “front end” with an RPA solution? Unfortunately, off the shelf RPA platforms are not sophisticated enough to handle the complexities of EHRs. That’s why Smartlink Health Solutions created an integration platform as a service (iPaaS) with RPA capabilities specifically designed to work with EHRs. By leveraging the user interface (UI), Smartlink can extract or insert virtually any type of data, including unstructured data. This approach overcomes the limitations of API and database integrations but has some limitations of its own. For example, real-time EHR integration is not possible via the UI.
4 Common EHR Integration Challenges
1. Technical Limitations
Different EHR systems use different data formats and standards, making it difficult to share information seamlessly. This can lead to data duplication, errors, and delays in care. Additionally, different EHR vendors’ APIs vary greatly in the data available for extraction and the capabilities for data to be inserted.
2. Workflow
Providers don’t always use EHRs in exactly the way that they are intended to be used. This results in structured data being entered in the wrong location, making it very difficult to exchange with other systems.
3. Cost
EHR integration can be very expensive, particularly for small practices. It can vary from $500 to more than $50,000, depending on the complexity of the integration and the EHR vendor.
4. Data Security and Privacy
Ensuring the privacy and security of patient data is of critical importance to prevent HIPAA violations. As a result, many organizations implement policies that make it difficult to share patient information.
EHR Integration Challenges
Technical Limitations
EHR vendors interpret interoperability standards differently.
Workflow Limitations
Providers don’t always put data where they are supposed to.
Cost Limitations
EHR integration can be very expensive, particularly for small practices.
Data Security
Data privacy policies often make it difficult to share patient data.

10 Best EHR Integration Companies
Smartlink Health provides a cutting-edge EHR integration platform as a service that excels in custom bidirectional data exchange. Known for its versatility, Smartlink Data Connector (SDC) offers integration via APIs, HL7, direct database, and RPA, making it a comprehensive solution for various healthcare settings. Because of its unique ability to integrate with EHRs via the user interface, Data Connector overcomes the limitations of both APIs and database integrations. For example, it can insert unstructured data into a patient note or create a task. Smartlink also has the unique ability to parse and compare external data to EHR data and insert only critical discrete data that is missing in the EHR (like diagnoses, medications, and care gaps). With a focus on speed to implementation and zero effort for clinic staff, Smartlink Health ensures efficient data sharing and improved interoperability.
2. Pilotfish
Pilotfish provides innovative middleware solutions for EHR integration, aiming to simplify data exchange and connectivity challenges. With a focus on facilitating real-time data sharing and reducing implementation complexities, Pilotfish’s integration solutions cater to the evolving needs of healthcare organizations. The company is a viable choice for IT departments within healthcare organizations seeking an integration engine for constructing their integrations. Like other integration solutions, Pilotfish faces limitations imposed by EHR vendor APIs, restricting capabilities such as the extraction or insertion of unstructured data.
Interfaceware is widely recognized for its flagship product, Iguana. Iguana is an integration engine designed to facilitate the seamless exchange of healthcare data among disparate systems. It serves as a middleware solution connecting various healthcare applications and data sources. The company also provides tools and features for streamlined interface development. This includes capabilities for designing, testing, and deploying interfaces, making it more accessible for healthcare IT professionals to create and manage data connections. Interfaceware is a good option for a healthcare organization’s IT department that needs an integration engine to build their own integrations. Like other integration solutions, Interfaceware is limited by EHR vendor APIs. For example, the ability to extract or insert unstructured data is limited.
4. Kno2
Kno2 positions itself as a health information network to connect healthcare organizations to each other, and is connected to a number of other health information systems. The company is currently pursuing QHIN designation under TEFCA. It is a cloud-based solution focused on facilitating interoperable patient document exchange between providers via connectivity to other national health information networks. Kno2 adheres to industry standards like HL7 and FHIR, ensuring compatibility with most healthcare systems. The company caters to larger healthcare organizations, and EHR vendor reach is limited compared to many other integration vendors. For organizations requiring broader interoperability functionality beyond document exchange, Kno2 might not be the best option.
Galen is a leading healthcare IT company offering a broad portfolio of technical and professional services to empower healthcare organizations and provider groups. They provide solutions for data migration, archival, and interoperability, ensuring seamless data flow between disparate systems. Galen develops custom applications and workflows to cater to specific organizational needs and improve process efficiency. The company provides a range of technical services, including data analytics, system maintenance, and network security, to optimize IT infrastructure. Their expertise might be more suited for larger healthcare organizations with complex IT needs, potentially leaving smaller entities seeking more budget-friendly options.
6. Ellkay
Ellkay is a leading healthcare data management company specializing in facilitating data exchange and interoperability between disparate healthcare systems. The company offers pre-built connectors for various EHR platforms and supports HL7 and FHIR standards. Additionally, they aggregate data from diverse sources, standardize it, and provide comprehensive analytics tools. Ellkay also provides expert consulting services to help healthcare organizations define their data management strategies, optimize workflows, and improve interoperability initiatives. The company initially focused on providing integration between laboratories and EHRs, and that is where they are still strongest. Overall, Ellkay is a strong player in the healthcare interoperability landscape. Their expertise might be better suited for integrating large, established healthcare systems, as their services might be costlier compared to interoperability companies focusing on specific aspects of interoperability. Like other integration solutions, Galen is also limited by EHR vendor APIs.
7. Rhapsody
Rhapsody was originally developed by Orion Health. The company name was changed to Lyniate in 2019 after the merger with Corepoint, but rebranded as Rhapsody again in 2023. Both Rhapsody Integration Engine and Carepoint Integration Engine focus on data exchange in healthcare. Rhapsody Integration Engine offers a broader range of interoperability capabilities than Carepoint, and is geared towards larger organizations. The solution can be deployed on premise, cloud, or a hybrid. It supports FHIR, HL7, and API. Overall, Rhapsody Integration Engine is a powerful and versatile solution for healthcare IT organizations. However, the comprehensive functionality, learning curve, and cost can be a bit overwhelming for smaller organizations with simpler interoperability needs. Like other integration solutions, Rhapsody is limited by EHR vendor APIs.
8. Redox Engine
Redox Engine is a prominent player in healthcare interoperability, providing a robust platform for EHR integration. Redox simplifies data exchange by offering a standardized API layer, allowing healthcare organizations to connect seamlessly with diverse applications and services. With a focus on scalability and a vast network of supported health systems, Redox streamlines integration efforts for improved data accessibility. The company started with an emphasis on Epic, where its capabilities perform the strongest. Like other interoperability companies, Redox is limited by EHR vendor APIs. For example, the ability to extract or insert unstructured data is limited.
9. Healthjump
Healthjump specializes in creating bridges between healthcare systems, enabling the secure exchange of patient data. The platform is designed to aggregate and integrate data from various sources within the healthcare ecosystem. Healthjump has the ability to extract standard API data from a large number of EHRs. It can also integrate with some on-premise EHRs via the database, and therefore, extract unstructured patient data from a handful of EHRs. Healthjump is more affordable than other interoperability companies like Redox. However, like other interoperability companies, Healthjump is limited by EHR vendor APIs, particularly for web-based EHRs. Additionally, Healthjump’s emphasis is on data extraction and aggregation, so its ability to insert data into EHRs is very limited without custom work, which is much more expensive than their “out of the box” standard integrations. Healthjump also cannot insert unstructured data into EHRs.
Zen Healthcare IT, often referred to simply as “Zen,” is a technology and consulting company focused on simplifying interoperability for healthcare organizations. They help healthcare providers, vendors, and other stakeholders overcome interoperability obstacles and create sustainable health information exchange (HIE) infrastructures. Zen’s flagship Gemini Integration Platform is a cloud-based IaaS solution that facilitates data exchange between disparate healthcare systems. It offers pre-built connectors, data mapping tools, and workflow automation capabilities. The company offers various consulting services, including interoperability strategy development, implementation support, and ongoing optimization of data exchange solutions.
Both Gemini and other Zen solutions prioritize user-friendliness, making them accessible to healthcare professionals without extensive technical expertise. While offering comprehensive solutions, Zen’s services might be costlier compared to other interoperability solutions. Their expertise might be better suited for large, established healthcare organizations with complex IT infrastructure and extensive data exchange needs. While offering pre-built connectors, some unique or niche healthcare systems might require additional customization or development by the client, requiring technical expertise.
If your team is ready for a solution that can address your EHR integration challenges, let's talk.
Contact us today at 877-502-3067 or info@smartlinkhealth.com.


